Immediate Functional Loading With Zygomatic Implants: The Graftless Solution For Patients With Severe Bone Loss
Dr. K. A REDDY: Department of Endodontics
Dr. SUGEETHIKA POLAPALA: Department of Public Health Dentistry
Ms. K. NIHARIKA REDDY
Dr. K. SHARADA REDDY
LBR Dental &Implant center, Hyderabad, India.
Corresponding Author: Dr. K.A REDDY
Available Online at: tijer.org/jnrid/papers/JNRID2503020.pdf
Abstract:
Severe maxillary bone loss presents significant challenges in dental rehabilitation, particularly in patients with systemic conditions like diabetes. Conventional bone grafting procedures often pose increased risks and prolonged treatment timelines. Zygomatic implants provide a graft less alternative, leveraging the dense Zygomatic bone for anchorage. This case report describes the successful rehabilitation of a 55-year-old female patient with severe maxillary atrophy using Zygomatic implants with immediate functional loading, following the CPBCCI protocol. The treatment eliminated the need for bone grafting, reduced morbidity, and ensured rapid restoration of function and aesthetics. The patient experienced significant improvement in quality of life with no postoperative complications. This report emphasizes the advantages of Zygomatic implants as a predictable solution for patients with compromised bone volume, particularly in medically compromised cases.
Index Terms
Zygomatic implants, Severe maxillary atrophy, Immediate functional loading, CPBCCI protocol, Diabetes management in dental implants, Quad Zygoma, Tubero-Pterygoid implants, Dental implants in India, Dental implant hospital India, Affordable teeth implants in India, Cost of dental implants in India, Periodontics and dental implants in India.
INTRODUCTION
Severe maxillary bone loss presents a significant challenge in dental rehabilitation, often resulting from trauma, tumor resection, congenital anomalies, or long-term edentulism with progressive resorption. Conventional treatment options, such as bone grafting and sinus augmentation, can be invasive, time-consuming, and associated with variable success rates.
Additionally, these approaches may not be feasible for patients with extensive bone deficiency or compromised systemic health.
Zygomatic implants have emerged as a revolutionary solution for managing severe maxillary atrophy without the need for bone grafting. Developed by Brånemark in the late 1990s, these extra-long implants anchor into the dense Zygomatic bone, providing a stable foundation for prosthetic rehabilitation. This technique has demonstrated high success rates, reduced morbidity, and shorter treatment timelines compared to traditional grafting procedures.
Immediate functional loading further enhances the benefits of Zygomatic implants. By providing provisional prostheses on the day of surgery, patients experience immediate functional and aesthetic improvements. This approach not only reduces the number of surgical interventions but also significantly improves patient satisfaction and quality of life.
The concept of a graft less solution eliminates the need for complex bone augmentation procedures, reducing the risk of surgical complications and expediting the overall treatment process. A better solution for this scenario, where the grafting surgery can be avoided, may be using an angulated screw channel technology which corrects the prosthetic screw access hole emergence in an alternative direction which is more aesthetic and acceptable.
Immediate functional loading further enhances the benefits of Zygomatic implants; by providing provisional prostheses on the day of surgery, patients experience immediate functional and aesthetic improvements. This approach not only reduces the number of surgical interventions but also significantly improves patient satisfaction and quality of life.
This case report highlights the successful management of a patient with severe maxillary bone loss using Zygomatic implants with immediate functional loading. The report emphasizes the surgical protocol, prosthetic rehabilitation, and clinical outcomes, contributing to the growing body of evidence supporting this graft less solution for complex maxillary rehabilitation.
MATERIALS & METHODS
CASE REPORT:
A 55-year-old female patient with a history of diabetes presented with complaint of mobility in her upper arch prosthesis and difficulty in chewing. The patient underwent root canal treatment following upper full-arch fixed partial denture (FPD) bridge seven years ago. On clinical examination, the FPD bridge was found to be mobile, and the patient reported discomfort during mastication.
Additionally, there was evidence of missing teeth in the lower right posterior region. Periodontal evaluation revealed generalized clinical attachment loss with probing depths of 6-7 mm. Radiographic examination using a panoramic radiograph showed severe maxillary bone loss with insufficient bone volume for implant placement. (figure 1)

Figure 1: Pre-Operative Panoramic Radiograph (OPG)
After a thorough evaluation, the decision was made to proceed with a graft less solution using Zygomatic implants. The CBCT analysis (figure 2) confirmed inadequate bone height in the anterior and posterior maxilla, making conventional implant placement without grafting impractical. Given the patient’s diabetic status, a bone grafting procedure posed a higher risk of delayed healing and infection.
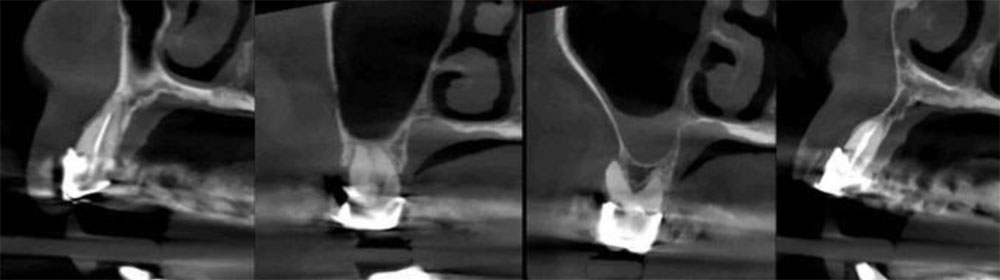
Figure 2: Preoperative CBCT images showing severe bone loss
Zygomatic implants offer a predictable alternative without the need for bone augmentation. They provide the advantage of immediate functional loading, allowing for quicker prosthetic rehabilitation and enhanced patient satisfaction. Zygomatic implants are well-documented for their long-term stability and high success rates in cases of severe atrophy.
In this case, we have incorporated Dr. K A Reddy’s CPBCCI Protocol™ which can eliminate these hurdles by utilizing the available dense cortical bone in the jaw, ensuring stable and immediate implant placement. The special design of the implants helps avoid problems like Peri implantitis, and is also safe in individuals with Diabetics and smokers. Considering the patient’s diabetic condition, the CPBCCI (Crestal Polished Bicortical Conventional Implants) protocol was chosen to ensure optimal healing, reduce infection risks, and promote successful Osseo Integration.
Based on these factors, a treatment plan involving the placement of Zygomatic implants with immediate functional loading was finalized. The patient was informed about the procedure, its advantages, and potential risks. Informed consent was obtained prior to proceeding with the treatment. This report further elaborates on the surgical procedure, prosthetic rehabilitation, and post-operative outcomes to demonstrate the effectiveness of Zygomatic implants as a graft less solution in complex cases.
The procedure began by administering local anesthesia i.e, lignocaine (2% adrenaline, 1:200,000) as a local anesthetic agent. All the necessary precautions were taken while operating the surgery. The upper arch 6 implants using the ‘All on 6 implants” were placed with (2 tubero Pterygoid implants, Quad Zygoma (4 Zygomatic implants, 2 on each side) and DMLS bridge screwed which required a standard torque of 40 ncm. In the lower arch, all 6 implants were placed bypassing the nerve and engaging the bicortical bone achieving a standard torque (Figure 3)
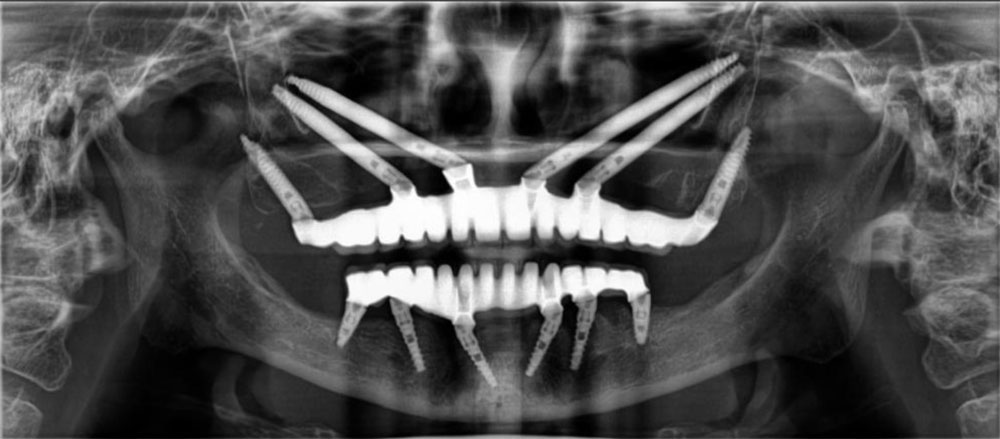
Figure 3: Post-Operative Panoramic Radiograph (OPG) Showing Quad Zygoma and TuberoPterygoid Implants with Immediate Prosthetic Loading after 1week follow-up.
After implants were placed, multi-unit abutments were positioned to ensure correct alignment and subsequent prosthetic rehabilitation. Implant supported fixed partial denture was employed using NORIS Abutment® Solutions system with angulation rectification by a graft less procedure.
On day 3, occlusal modifications were made if necessary, and sent back to prosthetic lab for further corrections. On Day 4, a cobalt chromium metal bar was fixed with DMLS teeth and trial was done to ensure final occlusal corrections. Putting on the impression caps and making the imprint, the metal trial was again sent back to the prosthetics lab. The patient’s occlusal records/jaw relations were noted and final prosthesis delivered to the patient on day 7.
Postoperative care:
Patients were instructed to take oral antibiotics [amoxicillin 500 mg + clavulanic acid 125 mg (625mg)] every 12 hours for five days and non-steroidal anti-inflammatory analgesics (Acecloplus) every eight hours for five days after surgery, as well as to apply cold fermentation intermittently and avoid rinsing or drinking hot beverages for 24 hours.
Outcomes:
The patient experienced a successful recovery with no postoperative complications. Immediate functional loading of the prosthesis significantly improved the patient’s chewing ability and aesthetics. Pain and discomfort were minimal, and no signs of infection or inflammation were observed at follow-up visits. Radiographic evaluation confirmed the stability and Osseo Integration of the implants. The patient expressed satisfaction with the final prosthesis, reporting restored confidence and improved quality of life. (figure 4)
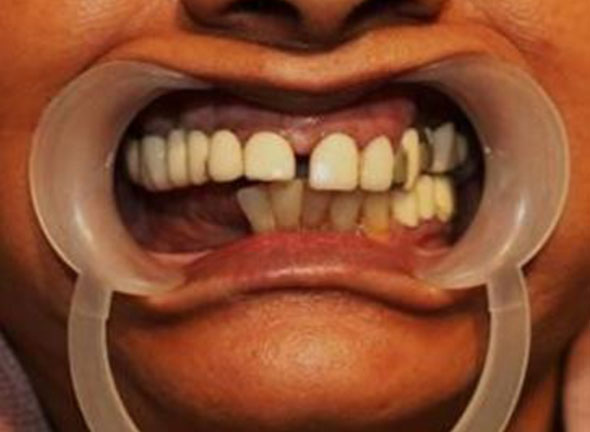
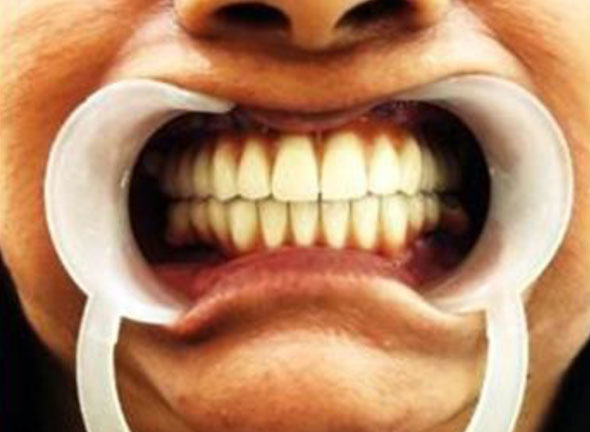
Figure 4: Pre- and Post-Operative Comparison of Full-Arch Rehabilitation with Zygomatic Implants
DISCUSSION
Zygomatic implants, especially when combined with the CPBCCI protocol, provide an effective graft less solution for patients with severe maxillary bone loss. In this case, the decision to avoid bone grafting minimized surgical morbidity and reduced the overall treatment time. The protocol’s emphasis on utilizing dense cortical bone for implant anchorage ensured primary stability, even in a patient with diabetes.
Immediate functional loading not only shortened the treatment timeline but also enhanced the patient’s psychological and functional well-being. Additionally, the use of a cobalt chromium bar with DMLS teeth ensured durability and aesthetic appeal. This approach is especially beneficial for diabetic patients where delayed healing is a concern. Furthermore, the CPBCCI protocol’s specialized design minimizes the risk of peri-implantitis, a common complication in diabetic and immune compromised patients.
CONCLUSION
This case report demonstrates the successful rehabilitation of a severely atrophic maxilla using Zygomatic implants with immediate functional loading, following the CPBCCI protocol. The graft less approach minimized treatment time and surgical complexity while ensuring predictable results. The patient achieved excellent functional and aesthetic outcomes, reinforcing the viability of this technique in similar cases. Further long-term follow-ups will continue to monitor implant stability and overall patient satisfaction.
Declaration by Authors
Ethical Approval: Approved
Acknowledgement: None
Source of Funding: None
Conflict of Interest: No conflicts of interest declared.
REFERENCES
- Brånemark PI, Gröndahl K, Ohrnell LO, Nilsson P, Thomsen P, Wennström J, et al. Rehabilitation of severely resorbed maxillae using extra-maxillary anchorage implants in the zygomatic bone: Preliminary results from a prospective clinical follow-up study. Clin Implant Dent Relat Res. 2004;6(1):3-10.
- Aparicio C, Manresa C, Francisco K, Claros P, Alández J. Immediate/early loading with zygomatic implants: A systematic review of the survival rates. J Clin Periodontol. 2014;41(6):556-67.
- Chrcanovic BR, Abreu MH, Ragghianti MS, Munoz PP. Survival and complications of zygomatic implants: A systematic review. Oral Maxillofac Surg. 2013;17(2):81-93.
- Esposito M, Maghaireh H, Grusovin MG, Ziounas I, Worthington HV. Immediate loading of zygomatic implants for rehabilitation of the atrophic maxilla: A randomized controlled trial. Eur J Oral Implantol. 2012;5(3):233-44.
- Albrektsson T, Zarb G. The Brånemark osseointegrated implant: A historical perspective. J Prosthet Dent. 1986;55(4):448-54.
- González-Martín ML, Torres-Ruiz FM, Torres-Carranza E, Gutiérrez-Pérez JL, GutiérrezCorrales A. Relevant Aspects of the Dental Implant Design on the Insertion Torque, Resonance Frequency Analysis (RFA) and Micromobility: An In Vitro Study. J Clin Med.
2023 Feb 1;12(3):855




